Many doctors performing labiaplasties were never taught vulvar anatomy—leaving some patients scarred and unable to feel sexual pleasure.
Content warning for genital mutilation, medical trauma
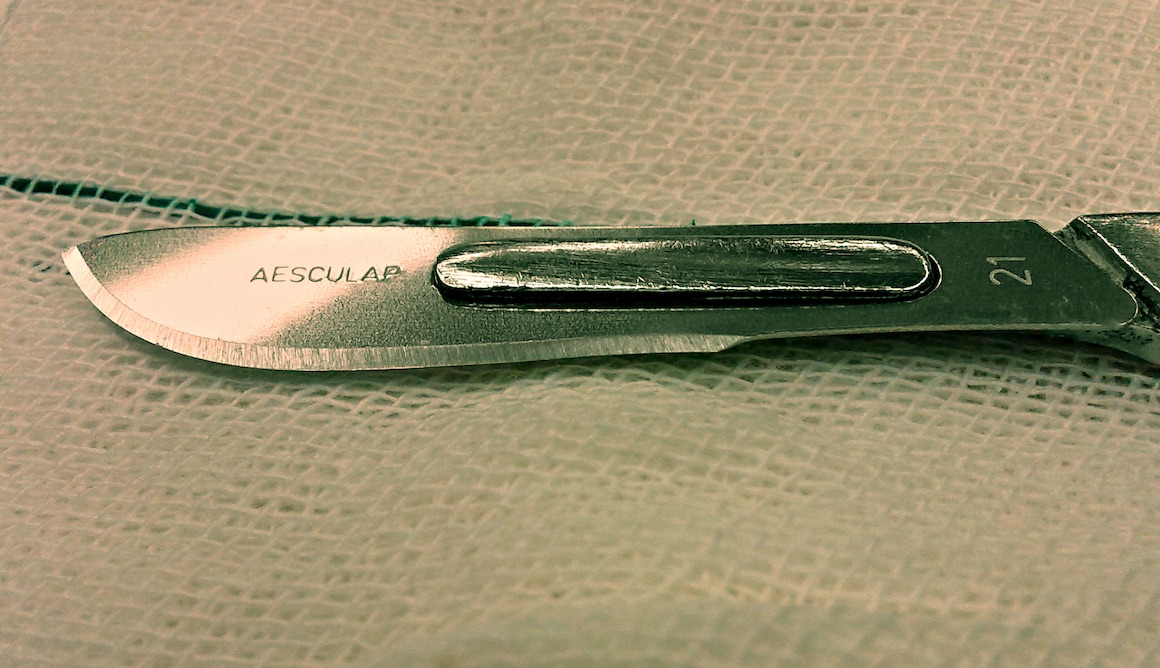
When Jessica Pin got a labiaplasty at age 18, her consent form read, “excision of redundant labia.” Instead, the doctor cut off the entirety of her labia minora and performed a clitoral hood reduction she never agreed to.
Afterward, when she touched her clitoris, there was no sensation. Since then, she hasn’t been able to orgasm, or feel much of anything at all, without a vibrator—something therapists and doctors dismissed as normal or a consequence of her “not being in love.”
When she wrote to her surgeon about what happened, he said he’d given her what she asked for. But an examination from his colleague confirmed that the dorsal nerve of her clitoris had been cut, leaving scars.
She wanted to report her surgeon, but her psychiatrist warned her that the board would defend him and attack her. Plus, the loss of her sexual functioning combined with the backlash she’d received for talking about it had left her suicidal. By the time she felt mentally healthy enough to speak out, the statute of limitations had passed. The doctor went on to win awards and become president of the state medical association. And even after she got yet another examination from his colleague, her surgeon said the scars must have been from a different surgery (which she never got) or that she must have done it herself (which she didn’t).
The loss of her sexual functioning combined with the backlash she’d received for talking about it left her suicidal. Click To TweetWhen another woman, who wishes to remain anonymous until her case goes to trial, got surgery to repair a tear to her labia after a sexual assault, she told the doctor not to go anywhere near her clitoris. “The doctor decided they needed to remodel my entire vulva, without discussing with me or asking for my consent, thinking this was best and would improve the ‘appearance,’” she remembers.
Instead of the minor repair she requested, her inner labia were completely cut off, and the skin of her outer labia and clitoral hood were pulled inward, causing nerve damage. In addition to losing all sexual sensation and ability to orgasm, she developed “extreme burning sensations, sharp pains in my clitoris glans, shaft, up the inguinal nerves and into my cervix.” She now finds it difficult to walk due to the pain. She had several consultations with doctors who do reconstructive surgery for botched labiaplasties. “They told me it looks like FGM,” she says.
A study she conducted that is currently awaiting publication has identified hundreds of women who have been victims of botched labiaplasties. Their complaints include complete amputation of the labia, inability to orgasm, clitoral injuries, and labia minora stitched to their labia majora, clitoral hood, or vagina.
It’s unclear how common incidents like these are, but they’re common enough that there are discussions on online forums dedicated to botched labiaplasties, as well as doctors who specialize in correcting them. One of them is Michael Goodman, MD, Clinical Assistant Professor in the Department of Obstetrics and Gynecology at the California Northstate University School of Medicine, who estimates that “well over a thousand” women suffer from botched labiaplasties each year. This number will likely grow, as labiaplasty is the world’s fastest-growing cosmetic surgery, seeing a 45% increase in 2016 alone.
They told me it looks like FGM. Click To TweetPin thinks this problem is more common than we realize because many victims are afraid to speak out. “Things got a lot worse for me when I started trying to talk about it and decided I needed to stand up for myself,” she says. “That’s why I suspect women who are harmed stay silent. The worst part was the gaslighting, victim-blaming, lying, and minimization.”
One reason labiaplasties get botched is that OB-GYNs don’t have an adequate understanding of the labia or clitoris, says Goodman. “OB-GYNs are both ’women’s surgeons’ and supposedly experts in vulvar and vaginal anatomy. They are trained to perform ulvovaginal procedures but receive absolutely no training in plastic procedures on the vulva,” he explains.
“While a board-certified plastic surgeon will not dare to perform a labiaplasty unless his or her residency program includes labiaplasty and genital anatomy in their training program, an (untrained in plastics) OB-GYN will think, ‘Well . . . how hard can it be? I am an expert in the vulva! Just cut it off and sew it up.’” Much of the issue could be solved through proper training in medical school and residencies, he says.
Paul Pin, MD, Chief of the Division of Plastic Surgery at Baylor University Medical Center, often trains residents who’ve been taught nothing about clitoral anatomy, and he’s never seen clitoral anatomy in plastic surgery journals. This means that many doctors who perform labiaplasties don’t even understand the body parts they’re operating on. Jessica’s doctor had only performed two labiaplasties and received no training in them.
Vulvar anatomy is also woefully absent in textbooks. After poring through medical books, Jessica has only been able to find the nerves and vasculature of the clitoris illustrated in two—Williams Gynecology and Williams Obstetrics—and even these didn’t have accompanying descriptions. Anatomy books include “very little detail about clitoral anatomy—certainly less than the penis,” confirms Paul Pin. “The real nerve supply to the clitoris is almost universally absent in textbooks.”
No one even knows how many of these procedures are done, much less what the outcomes are. Click To TweetAnother problem is that doctors who offer labiaplasties are not held accountable for providing the procedure safely, he adds.
“Most labiaplasties are done in doctor’s offices under local anesthesia, in non-certified operating rooms. No one even knows how many of these procedures are done, much less what the outcomes are. Professional societies should demand their members report their numbers and their outcomes to insure patient outcomes.”
But the issue goes deeper than lack of training or oversight. Underlying the erasure of vulvar genitalia from textbooks, journals, and medical schools is a societal neglect for female sexual pleasure and health. Many people still describe vulvar genitalia as the “vagina,” neglecting the clitoris and other sensitive external parts. In sex ed and biology classes, people learn about the role of vulvar anatomy in reproduction, not its potential for pleasure. As feminist author Peggy Orenstein put it in her TED Talk, kids “learn that boys have erections and ejaculations, and girls have periods and unwanted pregnancy.”
It’s this view of women as baby-making or man-pleasing machines, rather than human beings with their own desires and needs, that colors medical education. “For most medical students, the great majority of sex-ed-related learning has to do with reproductive anatomy and functioning, not pleasure,” explains sexologist Carol Queen, PhD. “The clitoris isn’t really directly relevant to this, and so the ‘inner workings’ (uterus, ovaries, fallopian tubes, etc.) often get more attention.”
As such, many women and gender variant folks themselves don’t learn the importance of the clitoris—or that the labia can also be sources of sexual pleasure. “I didn’t know my body or understand the significance of lost external sensation because I thought the magic was supposed to be inside the vagina,” says Jessica.
What A Fake ‘Female Orgasm’ Statistic Says About Gender Bias
In a society that considers women’s primary role in sex to be pleasing men, injuries that do not affect their ability to have penis-in-vagina intercourse are trivialized. “Female sexuality is objectified in the way it is approached. The vulva isn’t well described as an actively functional apparatus, which it is,” says Jessica.
“Do you think men would go to urologists who didn’t know the nerves and vasculature of the penis? Obviously not in a million years. But for some reason, women are comfortable with doctors who approach their vulvas as if they are non-functional, inanimate objects. ‘How vulvas work’ is not a subject of much consideration because women are ‘complicated’ and ‘emotional,’ not sexual.”
Compounding this problem is an overall neglect for sexual pleasure in the medical field, and a denial of the fact that pleasure is part of health. For example, women who don’t experience adequate sexual arousal may suffer from painful sex, which could lead to medical problems, Queen explains.
Queen believes surgeons should be required to inform their patients that, even when they’re performed properly, labiaplasties remove sensitive tissue and could result in some loss of sexual sensation. The same goes for hysterectomies, she adds. “While it can absolutely be medically necessary, it is often the case that patients aren’t informed that sexual sensations may change, and historically, doctors didn’t focus on retaining fully functional neurology when they removed a uterus.”
If vulvas got the same standard of care as noses, I’d be happy. Click To TweetWhen Jessica has written about her botched surgery, some have questioned why she got a labiaplasty in the first place, and implied that she was asking for it by going under the scalpel. But while she acknowledges that unrealistic beauty standards led her to get the surgery, she points out that other forms of surgery are held to higher standards, regardless of the patient’s motives. “If vulvas got the same standard of care as noses, I’d be happy,” she says.
Ultimately, if people learned about and valued women’s sexual anatomy and pleasure, fewer people would be getting labiaplasties, and those who did would be able to get them more safely, says Queen. “It’s not just that doctors need pleasure-inclusive sex education as part of the medical curriculum,” she says. “Everyone needs sex education that honors the fact that most people want sex that is pleasurable.”